Exploring post concussion syndrome
A concussion is a traumatic brain injury that affects one’s brain function. According to the world-renowned Mayo Clinic, in most cases, the effects of a concussion are temporary, including headaches and concentration problems.
On average, 1.1 million to 1.9 million children will get sports-related concussions. While most children recover within a few days to a few weeks, some only suffer from the physical aspect of symptoms for that short period of time. Yet approximately 10% of people who sustain a concussion will develop persisting-concussion syndrome (PCS).
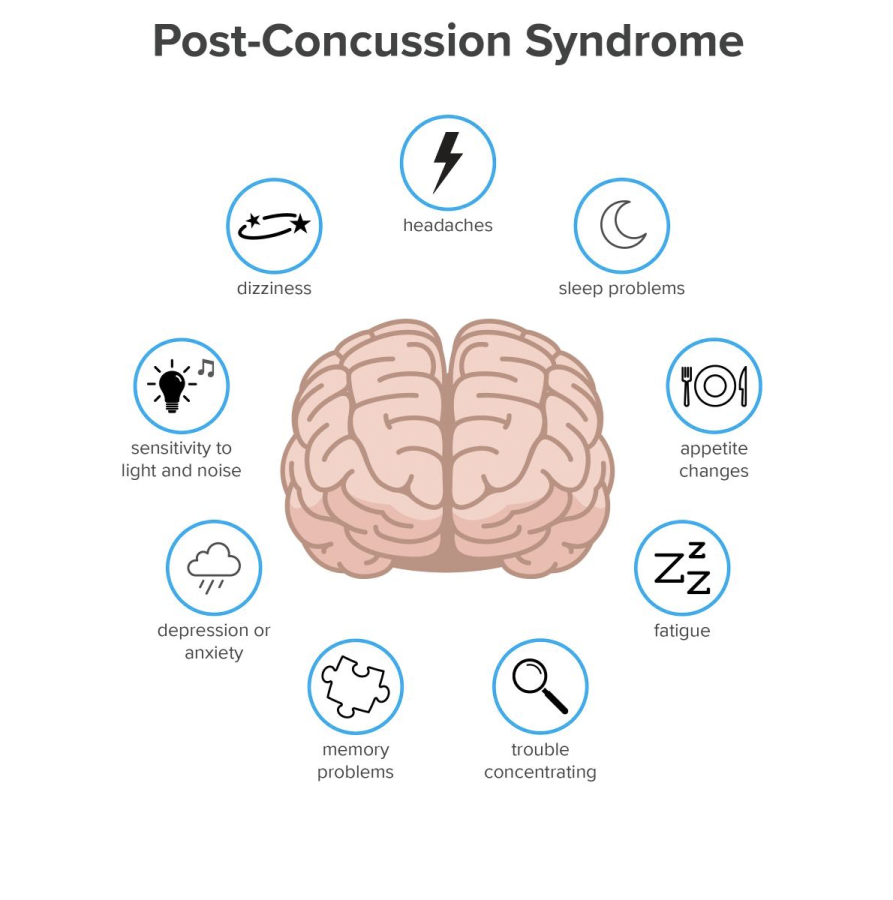
PCS symptoms often include cognitive, sleep, behavioral, and/or physical ailments. A study conducted through different Canadian Neurological programs aimed to evaluate the considerable number of concussion patients and the prevalence of clinical symptoms of anxiety and depression PCS. PCS can last for months, years, or even indefinitely and seriously impact our nation’s children. Growing concussion rates correlate with an increase in poor quality of life post-concussion, according to PCOM’s “Can Your Child’s Concussion Trigger Depression? Mood Swings? Suicide.”
Recent findings in the article above suggest that depression and anxiety in PCS can diminish the quality of life, not only as pain persists, but for the neurological impact a concussion has on one’s mental health. The outdated protocols for concussions can set up the perfect storm for depressive symptoms. This includes sitting in a dark room, lack of internet use, and no school.
The baseline feelings of sadness are expected after sustaining a concussion, as the symptoms themselves can impact one’s emotions. A traumatic brain injury (TBI) resource, Concussion Legacy Foundation, found that nearly two-thirds are affected by depression within seven years after injury.
For starters, depression may stem from injury to the areas of the brain affected upon impact. This includes parts of the brain that control emotions, along with a shift in levels of neurotransmitters, causing depression. Although some people inherit genes that pose a higher risk for depression, the influence of a concussion or TBI can feed the body’s natural incline to develop such a diagnosis.
Now, with thoughtful analysis of research, what can we do to help those in need?
While we can perform preventative measures, disengage in contact sports or wear protective gear, appropriate screening should address mental health concerns once a concussion occurs. Providing advocacy aids those in need to get the attention they need to continue a higher level of care. In a conjoined effort to address the source of the problem, the concussion, and follow up with mental health screenings and care, it is essential to address the risk factors for such mental illnesses post-concussion.
For more information and resources, visit https://concussionfoundation.org

Aside from always talking about her dog, Lauren Greenberg is always up for a good time. She is a senior at East and is in her fourth year involved in Eastside....